Transfusion medicine
Transfusion medicine handbook
The Transfusion Medicine Handbook is designed to assist hospital staff and other health professionals in modern Transfusion Medicine Practice.
4. Blood Components
4.8 Red Cell Components
ABO Compatibility
It is important that transfusion recipients receive red cell components compatible with their own ABO group. Incompatible transfusion can result in serious harm or death of the recipient.
It is best practice to transfuse donor red cells that are matched for the recipient. In some circumstances it may not be possible to transfuse the recipient with donor cells of the same group.
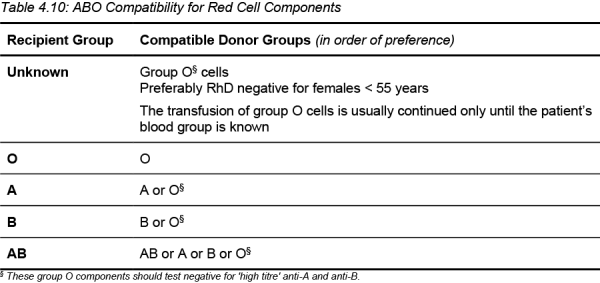
Table 4.10: ABO Compatibility for Red Cell Components outlines alternative donor groups that may be given to a recipient if supplies of ABO identical red cells are not available or are in short supply.
Table 4.10: ABO Compatibility for Red Cell Components
RhD Compatibility
Red cell and platelet transfusions are normally of the same RhD type as the patient. RhD negative components may be given to RhD positive recipients without any risk of immunisation.
In life-threatening situations it may be necessary to transfuse RhD negative recipients with RhD positive red cells. In these circumstances the blood bank will provide guidance. It is essential that the treating clinician is informed and the appropriateness of administration of prophylactic anti-D immunoglobulin considered.
If supplies of RhD negative red cells are low, RhD positive red cells may be provided by the blood bank for RhD negative males and for females beyond reproductive years.
In the case of RhD negative females with child-bearing potential, transfusion of RhD positive red cells must only be considered following discussion with a NZBS Transfusion Medicine Specialist.
Section 5.4.7: Rh(D) Immunoglobulin-VF contains guidelines on dosing of prophylactic anti-D following transfusion of RhD positive components.
Guidelines for Appropriate Use
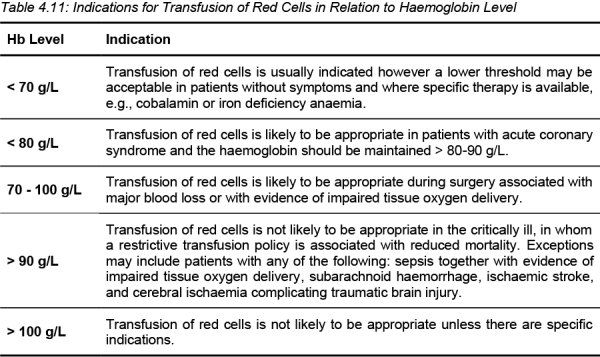
In deciding whether or not to transfuse red blood cells, the haemoglobin level should not be the sole deciding factor (see Table 4.11). Patient factors, signs and symptoms of hypoxia, ongoing blood loss, the degree of urgency required in correcting the anaemia and the risk of transfusion-related adverse effects should all be considered. The key issue is delivery of adequate amounts of oxygen to tissues. For a 70-80 kg patient, a transfusion of 4-5 mL/kg will increase the circulating haemoglobin by about 10 g/L.
Some specific factors to consider before deciding to transfuse:
- Cardiopulmonary reserve
If cardiac or pulmonary function is not normal, it may be necessary to consider transfusing at a higher haemoglobin level. - Volume of blood loss
Clinical assessment should attempt to quantify the volume of blood loss before, during, and after surgery, to ensure maintenance of adequate blood volume. - Oxygen consumption
This may be affected by a number of factors including fever, anaesthesia, shivering and thyrotoxicosis. If oxygen consumption is increased it may be necessary to consider transfusing at a higher haemoglobin level. - Atherosclerotic disease
Critical arterial stenosis to major organs, particularly the heart, may modify indications for the use of red cells.
Table 4.11: Indications for Transfusion of Red Cells in Relation to Haemoglobin Level
Restrictive Red Cell Transfusion Policy
The decision to transfuse should take into account the risks, benefits and alternatives available, and should not be based on haemoglobin level alone. With this in mind, increasingly restrictive transfusion policies are being implemented in a variety of clinical settings.
Policies aim to safely provide the minimum amount of blood required for an individual patient through setting appropriate transfusion triggers and, where indicated, encouraging assessment of the patient's clinical status after transfusion of each single unit of red blood cells before determining that further transfusion is required. Restrictive policies are supported by evidence from a number of clinical areas of improved or equivalent clinical outcomes after minimising exposure to allogeneic blood.
One such policy, the 2014 Australian NBA Single Unit Transfusion Guide, has been designed for use in stable, normovolaemic adult patients, in an inpatient setting, who do not have clinically significant bleeding.
