Transfusion medicine
Transfusion medicine handbook
The Transfusion Medicine Handbook is designed to assist hospital staff and other health professionals in modern Transfusion Medicine Practice.
4. Blood Components
4.9 Platelet Components
Transfused platelets should ideally be the same ABO and RhD groups as the recipients. If platelet stocks do not permit this, then ABO/RhD compatible should be selected see Table 4.12: ABO Compatibility for Platelet Components. This is relatively free of adverse reactions although antibodies in the transfused plasma may occasionally cause a haemolytic reaction or a transiently positive direct antiglobulin test (DAT).
Table 4.12: ABO Compatibility for Platelet Components
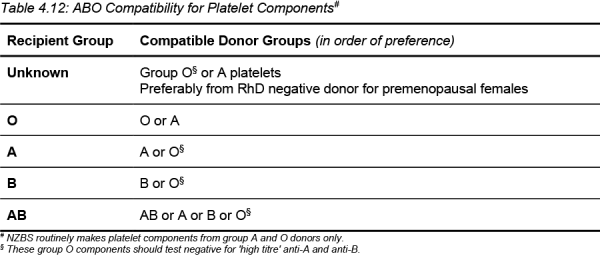
In life-threatening bleeding, ABO and/or RhD incompatible platelet components may be transfused.
RhD antigens are not expressed on platelets but red cells in RhD positive platelet components may sensitise RhD negative patients to form anti-D. When platelet components from a RhD positive donor are transfused into a RhD negative recipient, and in particular females with childbearing potential, administration of prophylactic anti-D immunoglobulin must be considered. Section 5.4.7: Rh(D) Immunoglobulin-VF contains guidelines on dosing of prophylactic anti-D following transfusion of RhD positive blood components.
Clinical Indications
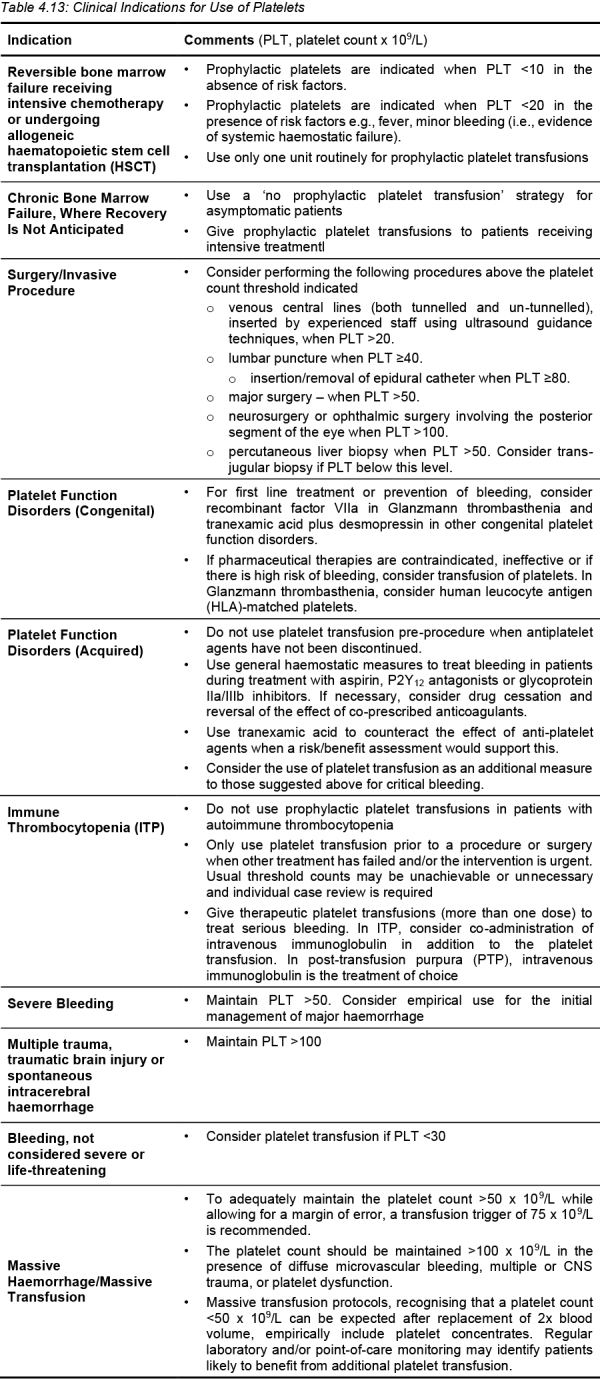
The 2016 BSH Guidelines for the use of platelet transfusions [3] provides some guidance that is summarised in Table 4.13. The BSH guideline on massive haemorrhage is also helpful [4] .
Table 4.13: Clinical Indications for Use of Platelets
Patients Refractory to Platelet Transfusion
A proportion of patients become refractory to random platelet transfusions. When a platelet transfusion fails to achieve the desired response, it is important to find out whether the failure is due to rapid immunological or non-immunological platelet consumption. Clinical factors such as sepsis, disseminated intravascular coagulation (DIC), and splenomegaly are more common than alloimmunisation as the cause of platelet refractoriness.
Identifying patients with antibodies to human leucocyte antigens (HLA) or human platelet antigens (HPA) is important since the use of HLA- or HPA-matched platelet components may result in improved transfusion response.
In deciding how to treat a refractory patient there may be a number of appropriate strategies for improving the response to platelet transfusions such as matching for HLA or HPA, increasing the transfused dose or even discontinuing transfusion.
NZBS has produced Guidelines for the Management of Patients Refractory to Platelets from which the table below is taken.
Table 4.14: Options for Managing Patients Refractory to Platelets

Matched platelets are prepared for a specific recipient after consultation with a NZBS Transfusion Medicine Specialist/ Medical Officer. Normally at least 48 hours’ notice is required because suitable donors need to be identified and attend to donate platelets. This is, followed by the usual pre-release testing for bacterial contamination. After transfusion a 30-minute platelet increment is indicated.
Contraindications
Transfusion of platelets is generally contraindicated in the following conditions:
- Thrombotic thrombocytopenic purpura (TTP)
- Haemolytic uraemic syndrome (HUS)
- Heparin-induced thrombocytopenia (HIT)
- Posttransfusion purpura (PTP)
Severe adverse reactions have been reported in patients with TTP and HIT following platelet transfusion. Platelet transfusion to these patients may also precipitate thrombotic events and can aggravate their clinical condition.
In this next group, platelet transfusion is unlikely to cause any sustained increase of platelet count:
- Immune thrombocytopenic purpura (ITP)
- Drug-induced thrombocytopenia of immune origin
Prophylactic use of platelet transfusion in these patients is of little benefit but platelet transfusion may be useful to stop active bleeding. Management of these complex disorders of haemostasis should involve a haematologist.
Adverse Reactions
Adverse reactions to platelets are predominantly allergic or febrile non-haemolytic transfusion reactions. The frequency of adverse reactions during transfusion of platelet concentrates has reduced following the introduction of platelet additive solution (PAS) as suspension medium.
